

Developing COVID-19 Care Expertise in Malawi
Preparing a hospital that serves more than 112,000 people from 70 surrounding villages for the COVID-19 pandemic was one of the hardest things Innocent Juma and his colleagues had faced in their careers. In Lunzu, Malawi, Innocent was just three years out of nursing school—and in his first posting at Mlambe Mission Hospital managed by the Daughters of Wisdom—when he had the daunting task of setting up and managing a COVID-19 screening system at the height of the pandemic.
At the beginning of the pandemic, health care workers all over the world were in the unusual situation of encountering a disease that was new to them. Medical personnel scrambled to understand the COVID-19 virus so they could provide the best care, prevention services and information to the communities who depended on them.
“At the height of the surge of COVID-19 in Malawi, we were seeing several positive cases a week, and I did not feel confident setting up a COVID screening tent or managing COVID-19 patients,” Innocent says.
Finding information

The hospital reception area in Mlambe Mission Hospital in Lunzu, Blantyre District, Malawi.
Photo by Dooshima Tsee/CRS
The Ministry of Health in Malawi provided three-day training sessions across the country to help health care providers like Innocent learn about COVID-19. The sessions were critical to laying a foundation of knowledge for managing COVID-19. However, the concepts were difficult to assimilate. As nurses and doctors put them into practice, they often encountered challenges and knowledge gaps that led to more questions. In addition, as COVID-19 infections increased and overwhelmed the system, staff were stretched and could not dedicate days to learning.
Felix Chuluota, the hospital administrator for Mlambe Mission Hospital, remembers the beginning of the pandemic as a time that was particularly trying for everyone. Felix has boundless energy and takes in his stride hospital emergencies like scarcity of masks and other personal protective equipment and staff shortages caused by the virus. He does this by thinking about future needs and planning as much as he can. However, a pandemic was something Felix could not have foreseen or planned for.
“It was a nightmare to train a hospital of 300 health professionals and still provide services as cases began to rise and our capacity was stretched,” he says. “When we got our first COVID-19 death, the nurses hadn’t been trained to handle [COVID 19-] positive body disposal and were coming to me for guidance. None of us knew what to do. I called around to other hospitals, but no one could help us. That was when I realized how alone we were and how desperately we needed training on all aspects of this disease,” says Felix.
A different approach to learning

Health care workers attend a training session in Mlambe Mission Hospital in Lunzu, Blantyre district, Malawi.
Photo: Dooshima Tsee/CRS
In 2020, Catholic Relief Services partnered with the European Union to create a blend of learning tools and methods for health care personnel to learn, ask questions and interact with colleagues from other countries and communities. This blended learning model focused on helping health care providers get the skills and information they needed to provide high quality services to COVID-19 patients as well as services to patients with pre-existing conditions that could make them more vulnerable to COVID-19.
Doctors, nurses and other health care staff joined multi-country and national virtual webinars and clinical case presentations. Internet connectivity was often an issue, so staff at the hospital gathered in a room and joined the virtual webinars using one connection. They also had off-site residential training sessions and simulations, on-the-job mentoring and self-directed learning.
“The weekly webinars and sessions were very helpful because we were able to take an hour to an hour and a half weekly rather than blocking out three days for learning. Also, we could ask questions, practice what we learned and come back with questions the next week,” Felix says.
Information to get the job done
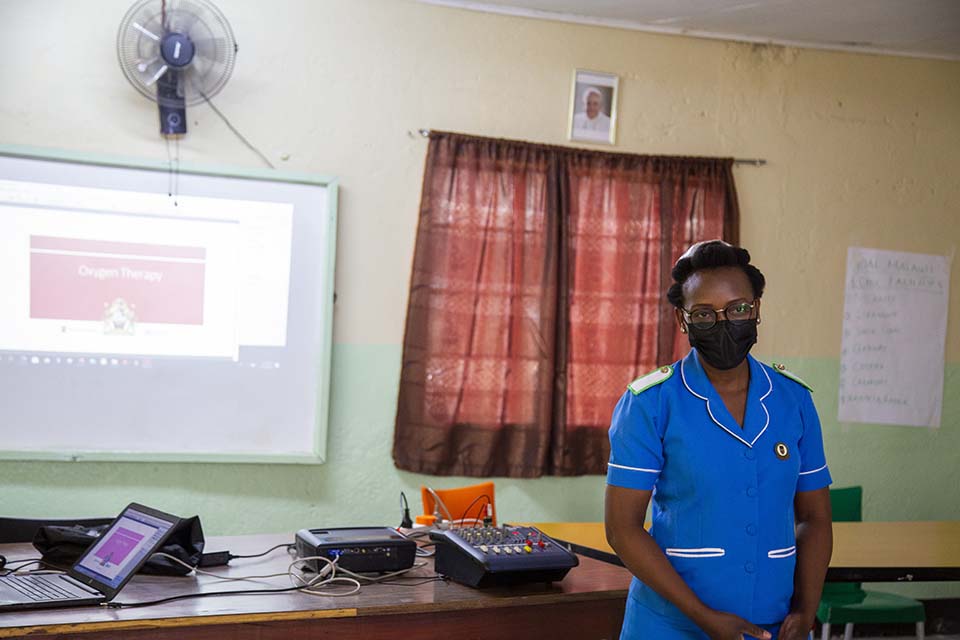
Miriam Makuta, deputy matron in charge of OBGYN, attends a training session in Mlambe in Lunzu, Blantyre district, Malawi.
Photo by Dooshima Tsee/CRS
The multi-country webinars gathered medical personnel from across southern Africa in a virtual space. For instance, cross learning provided the opportunity for nurses in Malawi to learn the methods that had worked in South Africa, Zambia or Madagascar—and vice versa.
Health personnel learned everything from the basics of COVID 19 prevention to more technical medical procedures. The basics included things like the proper way to wear a mask—because wearing a mask was suddenly something that not only health care staff needed to do. More complicated COVID-19 management concepts like resuscitating, administering oxygen, standard of care and required resources were also part of the training.
Mlambe Mission Hospital wasn’t a treatment center for COVID-19, but the hospital played a critical role: They were often the first point of call when people in the community started feeling unwell. Screening, accurate diagnosis, short-term management and referral for positive patients are lynchpins to prevent the spread of infection in the community and in hospitals.
Continuing professional development

IT staff set up connections and materials for a health care worker training in Mlambe Mission Hospital in Lunzu, Blantyre district, Malawi.
Photo by Dooshima Tsee/CRS
About 480 health care workers across 48 facilities in Malawi had access to the blended learning model, and between 40 and 70 health care workers joined each virtual webinar.
Rachel Thomas, a technical advisor, leads CRS’ COVID-19 response in Malawi. She believes the blended learning model worked particularly well because health care professionals had different entry points into the learning experience. Colleagues learning from each other proved an integral part of the model.
“While this model was used to build the capacity of health care professionals at district level for the COVID-19 response, I believe it is a learning model that can be used in any sector or topic as a method for continuing professional development for the partners we work with,” Rachel says.
Setting up a screening and referral system wasn’t easy. Having a community of colleagues across the world to learn with and learn from was both a relief and a source of confidence for Innocent and other health personnel in Mlambe Mission Hospital.
“The weekly training sessions gave us a blueprint to build our own screening and COVID-19 prevention and referral systems. We were able to organize testing, identify drugs and other needs to screen COVID-19 patients, and also prevent the virus from spreading within the hospital to other patients,” Innocent says.

